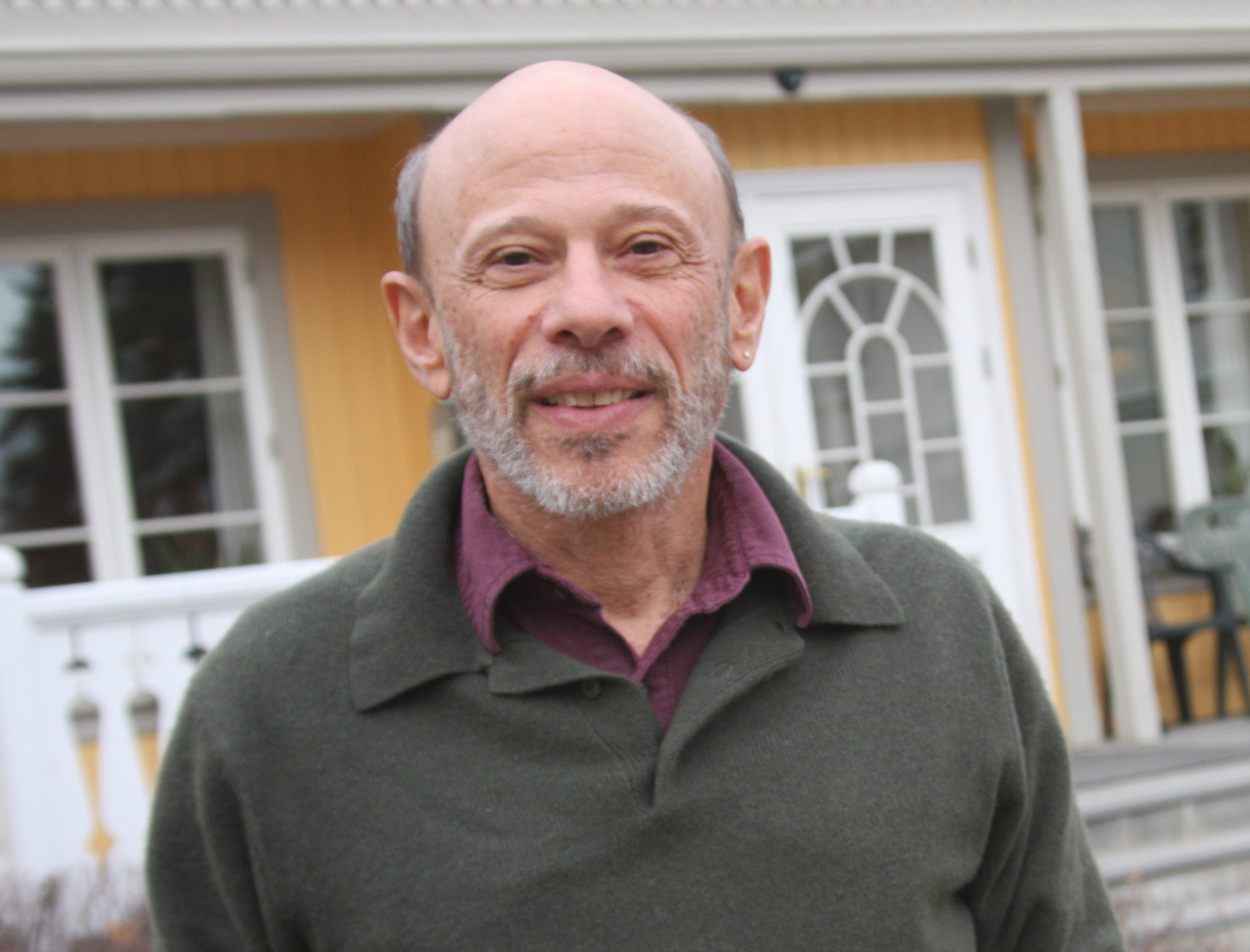
Greg Arnold: Bruce, you’ve been in the field of psychotherapy for over 30 years and have made a tremendous contribution to our understanding of psychotherapy from empirical, historical, and anthropological perspectives through what you call the “contextual model of psychotherapy.” Your fantastic book, The Great Psychotherapy Debate: The Evidence for What Makes Psychotherapy Work is in its second edition, and I highly recommend it to our readers.
I want to start right out with what I see as the most significant thing to share with our readers. In your research, you’ve found that the difference in effectiveness of various types of psychotherapy is zero percent. Is that right?
I want to start right out with what I see as the most significant thing to share with our readers. In your research, you’ve found that the difference in effectiveness of various types of psychotherapy is zero percent. Is that right?
Bruce Wampold: With some qualifications. I would put the differences between various types of psychotherapy at very close to zero percent. That statistic comes from clinical trials comparing treatment A to treatment B—often CBT to another form of CBT or to a dynamic therapy, a humanistic therapy, an interpersonal therapy—and there we don’t find any differences that are consistent or very large. Sometimes they’re small differences. The other area of research, “dismantling studies,” takes out the ingredient that is supposed to be the most important element of the treatment. It turns out that treatment is just as effective without the particular ingredient.
But here’s the qualification. There are a number of trials that compare a coherent, cogent, structured treatment to what’s often called “supportive therapy,” where the patient just sits with an empathic therapist, but there’s no treatment plan, there’s no explanation to the patient about what they’re going to do in therapy to help them get better. And we know, all the way back to Jerome Frank, that we need a coherent explanation for what’s bothering the patient and a believable treatment for them—something for the patient to do so that they work hard to overcome their difficulties. Supportive therapies are a lot more effective than doing nothing, but they’re not as effective for targeted outcomes as those that have a coherent explanation and treatment plan.
But here’s the qualification. There are a number of trials that compare a coherent, cogent, structured treatment to what’s often called “supportive therapy,” where the patient just sits with an empathic therapist, but there’s no treatment plan, there’s no explanation to the patient about what they’re going to do in therapy to help them get better. And we know, all the way back to Jerome Frank, that we need a coherent explanation for what’s bothering the patient and a believable treatment for them—something for the patient to do so that they work hard to overcome their difficulties. Supportive therapies are a lot more effective than doing nothing, but they’re not as effective for targeted outcomes as those that have a coherent explanation and treatment plan.
As long as what they’re doing is believable, accepted, is given by a therapist who’s skilled and believes in the treatment as well, the treatment tends to go well.
So if a patient comes in with problems in interpersonal relationships, depression, anxiety, we have to come up with a cogent explanation and a believable treatment to overcome their difficulties. As long as what they’re doing is believable, accepted, is given by a therapist who’s skilled and believes in the treatment as well, the treatment tends to go well.GA: Regardless of the treatment?
BW: That’s right. So that’s the long answer to your question about all treatments being equal. Of course, not all treatments are equal—there are harmful treatments. In my workshops, I show Bob Newhart doing “stop it” therapy.
GA: Yes, I’ve seen it. It’s hilarious.
BW: You can Google it on YouTube. He just keeps saying to the patient, “Stop it!” When we say all therapies are equally effective, we need to be clear that we are not talking about harmful or sarcastic therapy.
GA: Of course. So let’s take a case example, say someone with severe OCD. Most people think exposure with response prevention is far and away superior, its treatment rationale is better than anyone else’s treatment rationale, and that it’s the only therapy that will cure it.
BW: OCD is an interesting one to bring up.
The other thing about OCD is if you read the literature, outcomes are almost exclusively measured in terms of symptom reduction. There’s a failure to measure quality of life or interpersonal functioning. OCD is a terribly disturbing disorder, and the people who suffer from OCD often have a terrible quality of life—they’re isolated, they’re alienated from people, they’re not integrated into social networks because their disorder interferes, or they have other issues as well. So it’s very misleading to just measure targeted symptoms.
Exposure and response prevention is pretty good, with some provisos, but it’s never been compared to another bona fide, legitimate treatment for OCD.
Exposure and response prevention is pretty good, with some provisos, but it’s never been compared to another bona fide, legitimate treatment for OCD. I would like to see a focused dynamic treatment for OCD, and I would predict it doing just as well.The other thing about OCD is if you read the literature, outcomes are almost exclusively measured in terms of symptom reduction. There’s a failure to measure quality of life or interpersonal functioning. OCD is a terribly disturbing disorder, and the people who suffer from OCD often have a terrible quality of life—they’re isolated, they’re alienated from people, they’re not integrated into social networks because their disorder interferes, or they have other issues as well. So it’s very misleading to just measure targeted symptoms.
GA: It’s stacking the deck a little bit.
BW: I had a debate with a psychologist here in Wisconsin who has an OCD clinic, and he said the same thing: We know how to reduce symptoms. But the people are not back to work, they don’t have romantic or intimate relationships. So now we’re starting to augment the exposure and response prevention with vocational therapy and counseling for other issues. OCD is an area where we need to do more research.
The claims about CBT being superior to other treatments are not founded.
Another area where we thought CBT was the most effective treatment is panic disorder. But now Barbara Milrod and others have dynamic therapy for panic, and it’s just as effective. Social anxiety is another area. If you read the clinical trials carefully, there isn’t convincing evidence that one particular treatment is more effective. CBT folks have done some amazingly good research and have helped the field immeasurably. I don’t want to discount that, but the claims about CBT being superior to other treatments are not founded. GA: Those claims are far and wide, deeply rooted. Given that, among the bona fide treatments, they’re all equally effective, then the medical model is not superior either, correct?
BW: Yes. In Western culture, we’re so indoctrinated by the medical model that we ignore the social factors that make psychotherapy particularly effective. Humans are evolved as social animals, and we’re influenced through verbal means. How many of us learn not to stick our fingers in electric sockets because of classical conditioning? Our parents didn’t put our fingers into the socket to learn by experience, or put their fingers in there and have us watch them writhe on the floor in pain. All the parent had to do is say, “that’s dangerous.” We have evolved in such a way that significant others have tremendous influence on us through social means. Psychotherapy very effectively does just that.
A skilled therapist makes a big difference no matter the orientation.
The medical model can have some unfortunate consequences. It leads us to think that a “cure” can come through specific “interventions,” that if a therapist follows some kind of protocol, they will have good outcomes. That’s a myth. A skilled therapist makes a big difference no matter the orientation. GA: Which is good news, right? People are going to be happy to hear we make a difference.
BW:
Therapists Deteriorate Over Time
Yes, but it comes with responsibility. Let’s ensure that our outcomes are commendable, that they meet benchmarks, and that they improve. We just did a study where we looked at therapists over almost 20 years of practice, and the therapists did not improve. In fact, they deteriorated a bit.GA: Sobering.
BW: It is. But it’s not surprising when you think about it. What other profession do you go into a room, do your work in privacy, aren’t really allowed to talk about it because it’s confidential, and don’t get any feedback about how you’re doing. How can we expect to get better? Would we go to hear a musician who only performed and never practiced? Do you think world class tennis players just play Wimbledon and the U.S. Open and Australian Open? No, they practice hours a day on particular skills. So becoming a better therapist takes a lot of deliberate practice.
GA: Can you talk a little bit about the therapist factors that make us better or worse that we could be working on—be it in consultation groups or in feedback informed therapy.
BW: For many years I said the fundamental unanswered question in psychotherapy was, “What characterizes an effective therapist? What do they do?” And we didn’t know. But we’re starting to get good scientific evidence about what effective therapists do, so I’ll run through it.
GA: Please do!
BW: Effective therapists are able to form a working alliance—a collaborative working relationship—with a range of patients. The motivated patients with solid attachment histories who easily form an alliance with you—those aren’t the ones that challenge us. The ones that challenge us have poor attachment styles, do not have social networks, they alienate people in their lives, they have borderline features, they’re interpersonally aggressive, they tell us we’re no good. A really effective therapist is able to form a relatively good collaborative working relationship with those types of patients. The therapist effect is larger for more severely disturbed patients, which makes sense.
Effective therapists are also verbally fluent, they can describe the disorder as well as their treatment rationale.
Effective therapists are also verbally fluent, they can describe the disorder as well as their treatment rationale.
GA: They get the buy-in from the client.
BW: Yes, they’re persuasive as well as verbally fluent, so when they explain things, they do it in two or three sentences and it’s coherent. I have my students practice explaining what they’re going to do in therapy. It’s difficult to do and you have to practice until you can do it in three or four sentence.
An effective therapist can read the emotional state of clients even when they’re trying to hide it. And we know the patients hide what they’re feeling. It isn’t intentional; it’s part of their struggle in life. They suppress anger or they’re not allowed to express sadness. A good therapist can understand and respond to the patient affect. Good therapists also can modulate their own affect.
On the other hand, if we have an extremely anxious patient, can we be relaxed and calm? Modulating our own affect takes some practice as well. Are we warm, understanding, and caring? You may think all therapists are warm, understanding, and caring, but it takes work. I had a student whose patient didn’t bathe, so it reeked when the patient came in. What would your facial expression be?
An effective therapist can read the emotional state of clients even when they’re trying to hide it. And we know the patients hide what they’re feeling. It isn’t intentional; it’s part of their struggle in life. They suppress anger or they’re not allowed to express sadness. A good therapist can understand and respond to the patient affect. Good therapists also can modulate their own affect.
Can you be expressive and activated when you have a really depressed patient who just kind of sits there?
Can you be expressive and activated when you have a really depressed patient who just kind of sits there? Affect is really contagious. We know that from basic science.On the other hand, if we have an extremely anxious patient, can we be relaxed and calm? Modulating our own affect takes some practice as well. Are we warm, understanding, and caring? You may think all therapists are warm, understanding, and caring, but it takes work. I had a student whose patient didn’t bathe, so it reeked when the patient came in. What would your facial expression be?
GA: It would be hard not to feel some disgust.
BW: Exactly. We had to practice not displaying disgust. Being warm and empathic is easy with some patients, but really hard with others.
GA: Do people lose faith when they realize that the medical model, that any model really, isn’t the X factor in therapy? Do they just throw in the towel?
BW: I wouldn’t say that. When therapists say, “My treatment is the best there is for X, Y and Z,” in a way I’m glad. I want people to believe in their treatment, as that is an element of effective therapy. But instead of thinking that treatment X is the most effective treatment, we should believe that treatment X as I deliver it to this particular patient is effective.
This is where the focus on outcomes is so helpful. Is this patient getting better? Are they reaching their goals? If so, you can have faith not in the treatment itself but in your use of the treatment with the patient who is getting better. If we’re rigidly attached to a treatment, that’s problematic. I dislike it when therapists say in the first session, “Here’s how I work. This is what we’re going to do here.” You haven’t even listened to the patient yet and understood how the patient wants to work.
You need to modify treatment for some patients, or you might have to abandon it and do something very different for particular patients. Flexibility is another characteristic of effective therapists. That doesn’t mean doing something different every week with them, which is confusing; we need to be consistent, but also flexible.
This is where the focus on outcomes is so helpful. Is this patient getting better? Are they reaching their goals? If so, you can have faith not in the treatment itself but in your use of the treatment with the patient who is getting better. If we’re rigidly attached to a treatment, that’s problematic. I dislike it when therapists say in the first session, “Here’s how I work. This is what we’re going to do here.” You haven’t even listened to the patient yet and understood how the patient wants to work.
You need to modify treatment for some patients, or you might have to abandon it and do something very different for particular patients. Flexibility is another characteristic of effective therapists. That doesn’t mean doing something different every week with them, which is confusing; we need to be consistent, but also flexible.
GA: Dogma gets in the way here, and you’ve shown that more fidelity to a treatment actually gives less positive outcomes.
BW:
But there may be a crisis in a patient’s life or a dramatic event or they’re just resistant. One of the things I teach my trainees is to see the nonverbal signs of resistance—they’re not following through on activities or when we explain what we’re doing they look away. They don’t want to say, “No, that doesn’t make sense, you’ve got it wrong.” So we have to be really attuned to those signs and willing to explore them.
The Sweet Spot
There’s a sweet spot. You don’t want to be so flexible that you lack coherence, as that is not effective either. We need to be kind of in that sweet spot where there’s consistency in what we’re doing so the patient feels like we’re working towards their goals with a logical treatment plan.But there may be a crisis in a patient’s life or a dramatic event or they’re just resistant. One of the things I teach my trainees is to see the nonverbal signs of resistance—they’re not following through on activities or when we explain what we’re doing they look away. They don’t want to say, “No, that doesn’t make sense, you’ve got it wrong.” So we have to be really attuned to those signs and willing to explore them.
GA: Still, it seems like this contextual model kind of suggests that we don’t really need particular treatment models. That if we are naturally good at making alliances with all kinds of clients and verbally skilled, we don’t need to be steeped in a particular treatment model.
BW: Well that’s where coherence and clear articulation of a treatment plan come into play. You don’t have that without having some kind of approach. When we go to a doctor, we want to know what’s wrong with us and how we’re going to get better. CBT therapists are great at this. They incorporate psychoeducation into the treatment structure, so a coherent treatment plan is central to the work they do with clients.
Where CBT therapists can fall short if they don’t attend to it is the warm, empathic, understanding treatment expectation part of the contextual model.
Where CBT therapists can fall short if they don’t attend to it is the warm, empathic, understanding treatment expectation part of the contextual model.
If you administer CBT without warmth and understanding, it’s not going to be nearly as effective.
If you administer CBT without warmth and understanding, it’s not going to be nearly as effective. On the other side are the humanistic therapists who are often great at the warm, empathic part of therapy but don’t always have a coherent treatment structure. I think we all have to look at our practice and assess what we are really good at, what are the elements that seem to work well with our clients and then have a good hard look at the areas where we are falling short.GA: Yes, for me it’s figuring out the fine line between non-directive and directionless.
BW: That a good way to put it.
GA: It sounds like we should all be multi-modal, integrative, competent in several modalities because different things are going to work with different clients. None of us should be one-trick ponies.
To what extent does this call upon us to be more educated and trained in multiple modalities? Training culture these days seems to be trending towards manualized therapies, those that have been shown to be effective with particular disorders, etc. How do you think students should be getting trained these days?
To what extent does this call upon us to be more educated and trained in multiple modalities? Training culture these days seems to be trending towards manualized therapies, those that have been shown to be effective with particular disorders, etc. How do you think students should be getting trained these days?
BW: That’s an interesting question. I’m a counseling psychologist, and in counseling psychology we usually start by teaching the basic interpersonal skills first. In clinical programs, they are more often these days teaching manualized treatment—CBT for panic disorder or exposure therapy for OCD. We need to integrate the basic humanistic skills that are necessary for effective treatments as well as learning treatment protocols.
I have no problem with treatment protocols. I think people should be relatively fluent in several. And we should recognize our limitations. If we’re psychodynamic and have a client who is more interested in doing CBT, or we think would be better served by a CBT therapist, we should refer them out.
Look at how many treatment failures there are for widely accepted medical practices. We’re not going to help every psychotherapy patient, and maybe some other therapists could do a better job with particular patients. Flexibility is called for not just within a particular therapist, but within the community of therapists.
I have no problem with treatment protocols. I think people should be relatively fluent in several. And we should recognize our limitations. If we’re psychodynamic and have a client who is more interested in doing CBT, or we think would be better served by a CBT therapist, we should refer them out.
We often have this belief that we can help everybody, but it’s really not true.
We often have this belief that we can help everybody, but it’s really not true.Look at how many treatment failures there are for widely accepted medical practices. We’re not going to help every psychotherapy patient, and maybe some other therapists could do a better job with particular patients. Flexibility is called for not just within a particular therapist, but within the community of therapists.
GA: One of the elements of effective therapy you cited was being able to create a positive working alliance with a variety of patients, and difficult patients, so how do you balance that with knowing when to refer out?
BW: Well, the really effective therapists probably don’t refer out much because they’re pretty good at accommodating their treatment style to the particular patient. And we have to be careful about referrals because if it appears to the patient that they’re just being referred out because they’re difficult, that can be very wounding. I’ve heard of difficult patients saying, “I didn’t really get better, but this therapist stuck with me, and that was really helpful to me.”
Some disorders are going to take maintenance therapy to keep people out of the hospital and functioning. So even though they’re not going to approach what we would call “normal” functioning, it’s still an appropriate use of therapy. The medical model doesn’t really support this kind of treatment though. It’s looking for a specific outcome in a limited amount of time.
In the United States we’re paid by the health delivery system, which is advantageous for therapists because they’re getting paid, and advantageous for patients because there was a time when only the rich could pay out-of-pocket for therapy. Those without resources simply couldn’t afford psychotherapy and now it is available to many more people, which is a great thing. But there are some unfortunate consequences of being forced into this medical model. Limitations on sessions is probably the one that impacts therapists and clients the most.
Some disorders are going to take maintenance therapy to keep people out of the hospital and functioning. So even though they’re not going to approach what we would call “normal” functioning, it’s still an appropriate use of therapy. The medical model doesn’t really support this kind of treatment though. It’s looking for a specific outcome in a limited amount of time.
In the United States we’re paid by the health delivery system, which is advantageous for therapists because they’re getting paid, and advantageous for patients because there was a time when only the rich could pay out-of-pocket for therapy. Those without resources simply couldn’t afford psychotherapy and now it is available to many more people, which is a great thing. But there are some unfortunate consequences of being forced into this medical model. Limitations on sessions is probably the one that impacts therapists and clients the most.
GA: This isn’t going to change overnight. It’s deeply embedded in our culture. But in order to change the culture, we need a positive vision for the alternative. What would that look like? I think the contextual model has the potential to really change the system because not only is it scientific, it’s more scientific than the medical model.
BW: That’s a fundamental question we have to address.
We know psychotherapy is remarkably effective. It helps many people. It’s as effective as medication, and longer lasting. But we have to influence policy makers.
Many of us are working hard to influence policy, and the way to do that in my view is to present the evidence. I’ve dedicated my career to providing the evidence for the humane delivery of mental health services. We know psychotherapy is effective. It’s remarkably effective. It helps many people. It’s as effective as medication, and longer lasting. But we have to influence policy makers. There are places where we’re making progress, and there are places where it’s frustrating as hell.GA: I bet.
BW: But we also have to be making progress as therapists. We have a responsibility to provide effective services.
GA: It’s disheartening to hear that we aren’t getting better over the course of our own professional lives.
BW:
Coming Out of Isolation
We don’t, but as we learn more through research about what makes therapists effective, we can begin to incorporate what we learn into our training and professional development. I’m involved in a start-up company, TheraVue that’s dedicated to online skill building for psychotherapists. I think technology can play an important role in making not just therapy, but consultation and training more accessible to people.GA: That’s hopeful to hear. So many people want to be in consultation groups, but it’s much harder to make happen than you would think.
BW: This is an isolating profession. We’re sitting one-on-one or sometimes with couples or families, but essentially we’re doing our work in isolation. We have to have that peer support to help us both fight the isolation and to get better, but it’s difficult. We work six, eight hours a day with patients and at the end of the day, we don’t want to drive somewhere for a peer consultation. We want to get home to our families and friends.
GA: So given that there are these challenges, how do we get more therapists to make consultation a regular part of the practice?
BW: Psychotherapy is not the road to riches. I think most of us are in this field because we’re dedicated to helping people, so I think there’s an intrinsic motivation to get better. I don’t think there’s going to be resistance when people really understand what it takes to be a better therapist. In fact, there’s going to be eagerness to improve if it’s built-in in a way that makes it accommodating. I think it’s absurd that we don’t give CE units for actual efforts to improve other than going to workshops and doing online courses. I’m a licensed psychologist, so I do them, and some of them are really good, but is this helping me become a more effective therapist? Tomorrow are my patients going to be getting better therapy than they got before I went to this workshop? So the training and accreditation processes need to support the activities that actually help therapists get better.
GA: So we know that workshops and online courses and reading books isn’t enough. We recently did an interview with Tony Rousmaniere on deliberate practice, although we haven’t published this yet. It’s a concept he learned from Scott Miller that involves literally practicing—like tennis players do between games—the skills of therapy outside of the therapy office. Videotaping ourselves, practicing how we talk, having mentors watch our work, trying to eliminate things that aren’t helping clients—weird idiosyncrasies we wouldn’t necessarily pick up without an outside observer. Are these the kinds of practices you are talking about?
BW:
Good Therapists Are Humble
Yes, exactly. You can’t just reflect and think about your practice, just do process notes or whatever. It’s important to do those things, and certainly one of the characteristics of effective therapists is professional humility. Good therapists, the ones that get better outcomes, are the ones who say, “I’m not sure I’m helping patients. I need to get better.” But Daryl Chow and Scott Miller did a study that revealed that people who work outside of their practice to get better actually have better outcomes.Good therapists, the ones that get better outcomes, are the ones who say, “I’m not sure I’m helping patients. I need to get better.”
The skills I’ve talked about, you have to do them over and over again with feedback from somebody. This is what we’re doing with practicum students now. Often students will go, “I’m an advanced student now; these are basic skills you’re teaching.” No, we all need to practice these things. By the end, they often say, “this was the best practice class I’ve ever had because we actually practiced the skills we use in therapy.”GA: So we can improve our skills through practice, get unambiguous feedback from someone we respect and hopefully challenge our own confirmation bias that we’re the best therapist ever, by cultivating some humility.
Still, if the motivation to get better was intrinsic, don’t you think more therapists would be doing these things? Sell us a little more on it if you don’t mind. Like, how much am I going to improve if I implement these new strategies?
Still, if the motivation to get better was intrinsic, don’t you think more therapists would be doing these things? Sell us a little more on it if you don’t mind. Like, how much am I going to improve if I implement these new strategies?
BW: That’s a great question. In my presentations I use the example of baseball. The difference between a 300 hitter and a 275 hitter is not very much. In fact, if you watch the poor hitter for two weeks, they may have more hits than the 300 hitter. But if you look over the career, the 300 hitter helps his team immensely more.
A small improvement by each therapist would have a tremendous impact and benefit to patients.
An incremental improvement doesn’t have to be dramatic, but it has a tremendous impact on the number of patients who benefit from psychotherapy. I can give you the facts and figures because I love math and statistics, but a small improvement by each therapist would have a tremendous impact and benefit to patients. It’s quite remarkable.GA: So that’s our call to action as a profession.
BW: Yes.
GA: We know what we need to do, the gains are there for the taking, and we need to keep pushing on policy to support those efforts. None of us are going to get rich doing it, but it’s hopeful that we can really make a difference as we improve and grow.
BW: I think it is hopeful. We have the strategies and the technology for continual improvement as therapists. Let’s get better. Let’s work at it. Let’s support each other. And let’s measure outcomes so that we know how we’re doing.
GA: That’s a whole other piece we hadn’t talked about: measuring outcomes.
BW: Yes, it’s very important. What the research seems to show is that at least for cases at risk for deterioration, feedback may improve outcomes. But it’s pretty clear that just getting feedback—this patient is improving; this patient is not—doesn’t help the therapist become more skilled.
But it is important to know if you’re actually helping patients, if you’re gradually improving over time. Look and see what types of patients you’re having difficulty with.
But it is important to know if you’re actually helping patients, if you’re gradually improving over time. Look and see what types of patients you’re having difficulty with.
GA: Routinely.
BW: Yes, and I would add that, in my experience, and I think the research supports this, discussing the feedback with patients is helpful. What it communicates to the patient is that you are improving and that their feedback actually matters to you. But it also makes it clear that the focus is on, “Are you getting better?” I want to know that continually. We should all be discussing with our patients how therapy is going and how we can change to more readily support their goals. That’s a tremendously powerful message when we discuss that with patients. If we’re not meeting the goals, what can we do differently? Some would call that client-informed, but all therapists are client-informed. To a large degree, we should all be discussing with our patients how therapy is going and how we can change to more readily support their goals.
GA: There’s also an indirect benefit in that it communicates care in a new way to the client, bringing them in on monitoring outcome.
BW: It’s not indirect. It’s direct. In the contextual model, we don’t minimize these things as indirect. This is deliberate.
GA: The meat and potatoes.
BW: Absolutely. The focus on patient progress is central to what we do.
GA: So we have a call to action for clinicians, one for policy makers, what about for psychotherapy researchers?
BW:
My plea to all researchers would be, if you’re going to do a clinical trial, please include a quality of life measure because I want to see that your treatment actually has a significant benefit to patients in the quality of their life.
My plea to all researchers would be, if you’re going to do a clinical trial, please include a quality of life measure because I want to see that your treatment actually has a significant benefit to patients in the quality of their life. That’s why they come to treatment. I don’t want to just see targeted symptoms are reduced and therefore your model is best for a particular disorder.GA: Any final words of wisdom you’d like to leave our readers from your years in the industry?
BW: I would say to therapists—to all of us—let’s work to get better, to continually improve over the course of our careers. It will benefit patients. It will benefit us. Our satisfaction with our work will improve as well. At this point in my career, I want to do whatever I can to help therapists do that.
GA: I am so grateful for the work you do, and I want everyone to go out and read your work so that we can all become better therapists.
BW: Thank you, Greg, it’s been such a pleasure talking to you.