The field of psychotherapy has been around for quite a while—well over 100 years. According to sociologists of science, a field only reaches “maturity” when there exists a consensus amongst those working in the field. Within psychotherapy, we have yet to reach that stage. Instead, psychotherapy is characterized by someone coming up with still another new form of therapy. What seems to be most revered is what is “new.” As therapy practitioners and researchers, we are therefore confronted with some important questions: Are we destined to continue to forget what we know and instead focus on what is new? Will it always be the case that we emphasize who, not what, is right? Will the field forever be characterized by “dogma eat dogma?” “Is there nothing about psychotherapy about which we can agree?
Having spent approximately 60 years teaching, researching, supervising, and practicing psychotherapy—and ruminating all these years about these questions—I believe that one day we will have answers to them. In the meantime, where do we stand? I would suggest that there are indeed a few things we have learned over the years from the convergence of both clinical observation and psychotherapy research that can provide a crude, if not basic understanding of a few points of agreement.
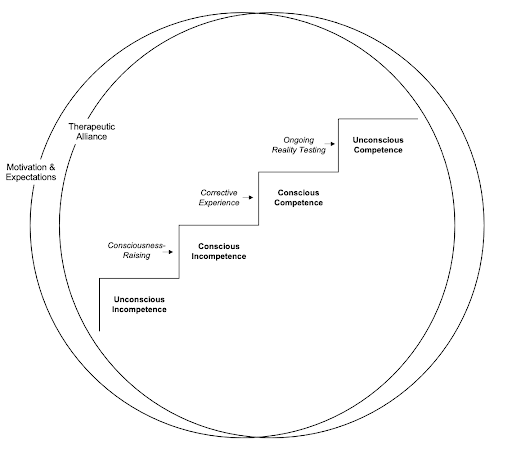
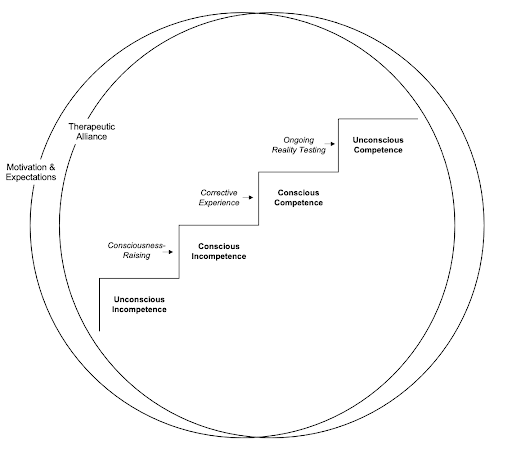
To begin with, if we step back and temporarily set aside our theoretical perspectives, it might be possible to say that most (all?) therapies proceed along somewhat similar stages of change. If effective, therapeutic change progresses as follows:
1. Unconscious Incompetence
2. Conscious Incompetence
3. Conscious Competence
4. Unconscious Competence
What does this mean? The patient comes in and says that there's something about their life that's not working, be it relational or symptomatic, but they don't know the factors that are contributing to this lack of effectiveness or incompetence. Thus, they are in an initial phase of unconscious incompetence.
As a result of the therapy—either what occurs in session or between-session self-observations—patients become more aware of the thoughts, actions, and/or emotions that may be creating problems in their life and contributing to their lack of competence. They may be misinterpreting what other people's motives are; not recognizing how their actions may be having a negative impact on others; becoming angry over not getting what they want instead of asking for something directly; and a host of other factors that are uncovered over the course of therapy. There are numerous ways that patients can come to understand why things are not working for them. Through the methods used to come to this understanding, they are now in the phase of conscious incompetence.
Becoming better aware of the reasons for their lack of effectiveness/competence may then lead to the need to function in a different way, taking into account those factors that are causing the lack of their intrapersonal or interpersonal competence. It is then that patients need to make deliberate efforts to behave, think, and/or feel differently: conscious competence.
If the therapy is successful, and over a period of time they benefit from numerous instances of corrective experiences, patients’ conscious competence may become more automatic, resulting in the final phase of unconscious competence.
In order to move patients through these phases, there are certain transtheoretical principles that cut across different schools of therapy.
None of this says anything about the specific techniques that different schools of therapy may use to implement the strategic principles, nor does it say anything about the overarching theoretical interpretation of why the interventions may work. At the level of abstraction that I have proposed, it clearly does not say it all. Still, it can provide the foundation for practice, training and research.
For those interested in learning more about this topic, I have written elsewhere on the topic. You can find these articles listed below.
__________
I would appreciate it if you could take this very brief survey (approximately 5 minutes) about transtheoretical principles of change: Please click here.
__________
Obtaining consensus in psychotherapy: What holds us back? — American Psychologist, Issue 74, pages 484-496
Consensus in psychotherapy: Are we there yet? — Clinical Psychology: Science and Practice, Issue 28, pages 267-276
File under: The Art of Psychotherapy, Musings and Reflections
Like what you are reading? For more stimulating stories, thought-provoking articles and new video announcements, sign up for our monthly newsletter.
Having spent approximately 60 years teaching, researching, supervising, and practicing psychotherapy—and ruminating all these years about these questions—I believe that one day we will have answers to them. In the meantime, where do we stand? I would suggest that there are indeed a few things we have learned over the years from the convergence of both clinical observation and psychotherapy research that can provide a crude, if not basic understanding of a few points of agreement.
To begin with, if we step back and temporarily set aside our theoretical perspectives, it might be possible to say that most (all?) therapies proceed along somewhat similar stages of change. If effective, therapeutic change progresses as follows:
1. Unconscious Incompetence
2. Conscious Incompetence
3. Conscious Competence
4. Unconscious Competence
What does this mean? The patient comes in and says that there's something about their life that's not working, be it relational or symptomatic, but they don't know the factors that are contributing to this lack of effectiveness or incompetence. Thus, they are in an initial phase of unconscious incompetence.
As a result of the therapy—either what occurs in session or between-session self-observations—patients become more aware of the thoughts, actions, and/or emotions that may be creating problems in their life and contributing to their lack of competence. They may be misinterpreting what other people's motives are; not recognizing how their actions may be having a negative impact on others; becoming angry over not getting what they want instead of asking for something directly; and a host of other factors that are uncovered over the course of therapy. There are numerous ways that patients can come to understand why things are not working for them. Through the methods used to come to this understanding, they are now in the phase of conscious incompetence.
Becoming better aware of the reasons for their lack of effectiveness/competence may then lead to the need to function in a different way, taking into account those factors that are causing the lack of their intrapersonal or interpersonal competence. It is then that patients need to make deliberate efforts to behave, think, and/or feel differently: conscious competence.
If the therapy is successful, and over a period of time they benefit from numerous instances of corrective experiences, patients’ conscious competence may become more automatic, resulting in the final phase of unconscious competence.
In order to move patients through these phases, there are certain transtheoretical principles that cut across different schools of therapy.
- To begin with, our patients need to have some degree of positive expectation and motivation that therapy will help. The most effective of therapies will not do anything if the patient's negative expectations and lack of motivation causes them to do nothing—or to terminate.
- There also needs to be the presence of an optimal therapeutic alliance. Much has been written about this, and there's both research evidence and clinical observations that this is an important transtheoretical principle.
- Helping patients to become better aware of themselves and their world can be implemented clinically in varying ways, depending on one’s theoretical approach and individualized case formulation.
- A most important principle of change involves encouraging the patient to try out new ways of functioning—corrective experiences—that help them become more effective emotionally, cognitively and behaviorally in their lives.
- Over the course of effective therapy, there develops a synergistic reciprocity of having corrective experiences that enhances patients’ awareness resulting in an ongoing reciprocity between corrective experiences and increased awareness—a form of ongoing reality testing.
None of this says anything about the specific techniques that different schools of therapy may use to implement the strategic principles, nor does it say anything about the overarching theoretical interpretation of why the interventions may work. At the level of abstraction that I have proposed, it clearly does not say it all. Still, it can provide the foundation for practice, training and research.
For those interested in learning more about this topic, I have written elsewhere on the topic. You can find these articles listed below.
__________
I would appreciate it if you could take this very brief survey (approximately 5 minutes) about transtheoretical principles of change: Please click here.
__________
Obtaining consensus in psychotherapy: What holds us back? — American Psychologist, Issue 74, pages 484-496
Consensus in psychotherapy: Are we there yet? — Clinical Psychology: Science and Practice, Issue 28, pages 267-276
File under: The Art of Psychotherapy, Musings and Reflections






